| Hypertension | |
|---|---|
| Other names | Arterial hypertension, high blood pressure |
 | |
| Automated arm blood pressure meter showing arterial hypertension (shown by a systolic blood pressure 158 mmHg, diastolic blood pressure 99 mmHg and heart rate of 80 beats per minute) | |
| Specialty | Cardiology, Nephrology |
| Symptoms | None[1] |
| Complications | Coronary artery disease, stroke, heart failure, peripheral arterial disease, vision loss, chronic kidney disease, dementia[2][3][4] |
| Causes | Usually lifestyle and genetic factors[5] |
| Risk factors | Lack of sleep, excess salt, excess body weight, smoking, alcohol[1][5] |
| Diagnostic method | Resting blood pressure >130/80 mmHg[6] or >140/90 mmHg[7] |
| Treatment | Lifestyle changes, medications[8] |
| Frequency | 33% (all), 16% (diagnosed) (globally, 2019)[9][10] |
| Deaths | 10.4 million; 19% of deaths (globally, 2019)[9] |
| Part of a series on |
| Human body weight |
|---|
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated.[11] High blood pressure usually does not cause symptoms itself.[1] It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia.[2][3][4][12] Hypertension is a major cause of premature death worldwide.[13]
High blood pressure is classified as primary (essential) hypertension or secondary hypertension.[5] About 90–95% of cases are primary, defined as high blood pressure due to nonspecific lifestyle and genetic factors.[5] Lifestyle factors that increase the risk include excess salt in the diet, excess body weight, smoking, physical inactivity and alcohol use.[1][5] The remaining 5–10% of cases are categorized as secondary hypertension, defined as high blood pressure due to a clearly identifiable cause, such as chronic kidney disease, narrowing of the kidney arteries, an endocrine disorder, or the use of birth control pills.[5]
Blood pressure is classified by two measurements, the systolic (first number) and diastolic (second number) pressures.[1] For most adults, normal blood pressure at rest is within the range of 100–140 millimeters mercury (mmHg) systolic and 60–90 mmHg diastolic.[6][7] For most adults, high blood pressure is present if the resting blood pressure is persistently at or above 130/80 or 140/90 mmHg.[5][6][7] Different numbers apply to children.[14] Ambulatory blood pressure monitoring over a 24-hour period appears more accurate than office-based blood pressure measurement.[5][11]
Lifestyle changes and medications can lower blood pressure and decrease the risk of health complications.[8] Lifestyle changes include weight loss, physical exercise, decreased salt intake, reducing alcohol intake, and a healthy diet.[5] If lifestyle changes are not sufficient, blood pressure medications are used.[8] Up to three medications taken concurrently can control blood pressure in 90% of people.[5] The treatment of moderately high arterial blood pressure (defined as >160/100 mmHg) with medications is associated with an improved life expectancy.[15] The effect of treatment of blood pressure between 130/80 mmHg and 160/100 mmHg is less clear, with some reviews finding benefit[6][16][17] and others finding unclear benefit.[18][19][20] High blood pressure affects 33% of the population globally.[9] About half of all people with high blood pressure do not know that they have it.[9] In 2019, high blood pressure was believed to have been a factor in 19% of all deaths (10.4 million globally).[9]
Signs and symptoms
[edit]Hypertension is rarely accompanied by symptoms.[1] Half of all people with hypertension are unaware that they have it.[9] Hypertension is usually identified as part of health screening or when seeking healthcare for an unrelated problem.
Some people with high blood pressure report headaches, as well as lightheadedness, vertigo, tinnitus (buzzing or hissing in the ears), altered vision or fainting episodes.[21] These symptoms, however, might be related to associated anxiety rather than the high blood pressure itself.[22]
Long-standing untreated hypertension can cause organ damage with signs such as changes in the optic fundus seen by ophthalmoscopy.[23] The severity of hypertensive retinopathy correlates roughly with the duration or the severity of the hypertension.[21] Other hypertension-caused organ damage include chronic kidney disease and thickening of the heart muscle.[9]
Secondary hypertension
[edit]Secondary hypertension is hypertension due to an identifiable cause, and may result in certain specific additional signs and symptoms. For example, as well as causing high blood pressure, Cushing's syndrome frequently causes truncal obesity,[24] glucose intolerance, moon face, a hump of fat behind the neck and shoulders (referred to as a buffalo hump), and purple abdominal stretch marks.[25] Hyperthyroidism frequently causes weight loss with increased appetite, fast heart rate, bulging eyes, and tremor. Renal artery stenosis may be associated with a localized abdominal bruit to the left or right of the midline, or in both locations. Coarctation of the aorta frequently causes a decreased blood pressure in the lower extremities relative to the arms, or delayed or absent femoral arterial pulses. Pheochromocytoma may cause abrupt episodes of hypertension accompanied by headache, palpitations, pale appearance, and excessive sweating.[25]
Hypertensive crisis
[edit]Severely elevated blood pressure (equal to or greater than a systolic 180 mmHg or diastolic of 120 mmHg) is referred to as a hypertensive crisis.[26] Hypertensive crisis is categorized as either hypertensive urgency or hypertensive emergency, according to the absence or presence of end organ damage, respectively.[27][28]
In hypertensive urgency, there is no evidence of end organ damage resulting from the elevated blood pressure. In these cases, oral medications are used to lower the BP gradually over 24 to 48 hours.[29]
In hypertensive emergency, there is evidence of direct damage to one or more organs.[30][31] The most affected organs include the brain, kidney, heart and lungs, producing symptoms which may include confusion, drowsiness, chest pain and breathlessness.[29] In hypertensive emergency, the blood pressure must be reduced more rapidly to stop ongoing organ damage;[29] however, there is a lack of randomized controlled trial evidence for this approach.[31]
Pregnancy
[edit]Hypertension occurs in approximately 8–10% of pregnancies.[25] Two blood pressure measurements six hours apart of greater than 140/90 mmHg are diagnostic of hypertension in pregnancy.[32] High blood pressure in pregnancy can be classified as pre-existing hypertension, gestational hypertension, or pre-eclampsia.[33] Women who have chronic hypertension before their pregnancy are at increased risk of complications such as premature birth, low birthweight or stillbirth.[34] Women who have high blood pressure and had complications in their pregnancy have three times the risk of developing cardiovascular disease compared to women with normal blood pressure who had no complications in pregnancy.[35][36]
Pre-eclampsia is a serious condition of the second half of pregnancy and following delivery characterised by increased blood pressure and the presence of protein in the urine.[25] It occurs in about 5% of pregnancies and is responsible for approximately 16% of all maternal deaths globally.[25] Pre-eclampsia also doubles the risk of death of the baby around the time of birth.[25] Usually there are no symptoms in pre-eclampsia and it is detected by routine screening. When symptoms of pre-eclampsia occur the most common are headache, visual disturbance (often "flashing lights"), vomiting, pain over the stomach, and swelling. Pre-eclampsia can occasionally progress to a life-threatening condition called eclampsia, which is a hypertensive emergency and has several serious complications including vision loss, brain swelling, seizures, kidney failure, pulmonary edema, and disseminated intravascular coagulation (a blood clotting disorder).[25][37]
In contrast, gestational hypertension is defined as new-onset hypertension during pregnancy without protein in the urine.[33]
Children
[edit]Failure to thrive, seizures, irritability, lack of energy, and difficulty in breathing[38] can be associated with hypertension in newborns and young infants. In older infants and children, hypertension can cause headache, unexplained irritability, fatigue, failure to thrive, blurred vision, nosebleeds, and facial paralysis.[38][39]
Causes
[edit]Primary hypertension
[edit]Hypertension results from a complex interaction of genes and environmental factors. Numerous common genetic variants with small effects on blood pressure have been identified[40] as well as some rare genetic variants with large effects on blood pressure.[41] Also, genome-wide association studies (GWAS) have identified 35 genetic loci related to blood pressure; 12 of these genetic loci influencing blood pressure were newly found.[42] Sentinel SNP for each new genetic locus identified has shown an association with DNA methylation at multiple nearby CpG sites. These sentinel SNP are located within genes related to vascular smooth muscle and renal function. DNA methylation might affect in some way linking common genetic variation to multiple phenotypes even though mechanisms underlying these associations are not understood. Single variant test performed in this study for the 35 sentinel SNP (known and new) showed that genetic variants singly or in aggregate contribute to risk of clinical phenotypes related to high blood pressure.[42]
Blood pressure rises with aging when associated with a western diet and lifestyle and the risk of becoming hypertensive in later life is significant.[43][44] Several environmental factors influence blood pressure. High salt intake raises the blood pressure in salt sensitive individuals; lack of exercise and central obesity can play a role in individual cases. The possible roles of other factors such as caffeine consumption,[45] and vitamin D deficiency[46] are less clear. Insulin resistance, which is common in obesity and is a component of syndrome X (or the metabolic syndrome), also contributes to hypertension.[47]
Events in early life, such as low birth weight, maternal smoking, and lack of breastfeeding may be risk factors for adult essential hypertension, although the mechanisms linking these exposures to adult hypertension remain unclear.[48] An increased rate of high blood uric acid has been found in untreated people with hypertension in comparison with people with normal blood pressure, although it is uncertain whether the former plays a causal role or is subsidiary to poor kidney function.[49] Average blood pressure may be higher in the winter than in the summer.[50] Periodontal disease is also associated with high blood pressure.[51]
Secondary hypertension
[edit]Secondary hypertension results from an identifiable cause. Kidney disease is the most common secondary cause of hypertension.[25] Hypertension can also be caused by endocrine conditions, such as Cushing's syndrome, hyperthyroidism, hypothyroidism, acromegaly, Conn's syndrome or hyperaldosteronism, renal artery stenosis (from atherosclerosis or fibromuscular dysplasia), hyperparathyroidism, and pheochromocytoma.[25][52] Other causes of secondary hypertension include obesity, sleep apnea, pregnancy, coarctation of the aorta, excessive eating of liquorice, excessive drinking of alcohol, certain prescription medicines, herbal remedies, and stimulants such as coffee, cocaine and methamphetamine.[25][53] Arsenic exposure through drinking water has been shown to correlate with elevated blood pressure.[54][55] Depression was also linked to hypertension.[56] Loneliness is also a risk factor.[57] Air pollution may be associated with hypertension.[58]
A 2018 review found that any alcohol increased blood pressure in males while over one or two drinks increased the risk in females.[59]
Pathophysiology
[edit]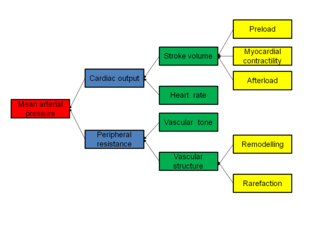
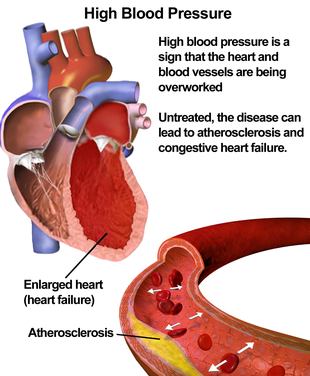
In most people with established essential hypertension, increased resistance to blood flow (total peripheral resistance) accounts for the high pressure while cardiac output remains normal.[60] There is evidence that some younger people with prehypertension or 'borderline hypertension' have high cardiac output, an elevated heart rate and normal peripheral resistance, termed hyperkinetic borderline hypertension.[61] These individuals develop the typical features of established essential hypertension in later life as their cardiac output falls and peripheral resistance rises with age.[61] Whether this pattern is typical of all people who ultimately develop hypertension is disputed.[62] The increased peripheral resistance in established hypertension is mainly attributable to structural narrowing of small arteries and arterioles,[63] although a reduction in the number or density of capillaries may also contribute.[64]
It is not clear whether or not vasoconstriction of arteriolar blood vessels plays a role in hypertension.[65] Hypertension is also associated with decreased peripheral venous compliance,[66] which may increase venous return, increase cardiac preload and, ultimately, cause diastolic dysfunction. For patients having hypertension, higher heart rate variability (HRV) is a risk factor for atrial fibrillation.[67]
Pulse pressure (the difference between systolic and diastolic blood pressure) is frequently increased in older people with hypertension.[68] This can mean that systolic pressure is abnormally high, but diastolic pressure may be normal or low, a condition termed isolated systolic hypertension.[69] The high pulse pressure in elderly people with hypertension or isolated systolic hypertension is explained by increased arterial stiffness, which typically accompanies aging and may be exacerbated by high blood pressure.[70]
Many mechanisms have been proposed to account for the rise in peripheral resistance in hypertension. Most evidence implicates either disturbances in the kidneys' salt and water handling (particularly abnormalities in the intrarenal renin–angiotensin system)[71] or abnormalities of the sympathetic nervous system.[72] These mechanisms are not mutually exclusive and it is likely that both contribute to some extent in most cases of essential hypertension. It has also been suggested that endothelial dysfunction and vascular inflammation may also contribute to increased peripheral resistance and vascular damage in hypertension.[73][74] Interleukin 17 has garnered interest for its role in increasing the production of several other immune system chemical signals thought to be involved in hypertension such as tumor necrosis factor alpha, interleukin 1, interleukin 6, and interleukin 8.[75]
Excessive sodium or insufficient potassium in the diet leads to excessive intracellular sodium, which contracts vascular smooth muscle, restricting blood flow and so increases blood pressure.[76][77] Non-modulating essential hypertension is a form of salt-sensitive hypertension, where sodium intake does not modulate either adrenal or renal vascular responses to angiotensin II.[78] They make up 25% of the hypertensive population.[79]
Diagnosis
[edit]Hypertension is diagnosed on the basis of a persistently high resting blood pressure. Elevated blood pressure measurements on at least two separate occasions is required for a diagnosis of hypertension.[6][7][13]
Measurement technique
[edit]For an accurate diagnosis of hypertension to be made, it is essential for proper blood pressure measurement technique to be used.[80] Improper measurement of blood pressure is common and can change the blood pressure reading by up to 10 mmHg, which can lead to misdiagnosis and misclassification of hypertension.[80] Correct blood pressure measurement technique involves several steps. Proper blood pressure measurement requires the person whose blood pressure is being measured to sit quietly for at least five minutes which is then followed by application of a properly fitted blood pressure cuff to a bare upper arm.[80] The person should be seated with their back supported, feet flat on the floor, and with their legs uncrossed.[80] The person whose blood pressure is being measured should avoid talking or moving during this process.[80] The arm being measured should be supported on a flat surface at the level of the heart.[80] Blood pressure measurement should be done in a quiet room so the medical professional checking the blood pressure can hear the Korotkoff sounds while listening to the brachial artery with a stethoscope for accurate blood pressure measurements.[80][81] The blood pressure cuff should be deflated slowly (2–3 mmHg per second) while listening for the Korotkoff sounds.[81] The bladder should be emptied before a person's blood pressure is measured since this can increase blood pressure by up to 15/10 mmHg.[80] Multiple blood pressure readings (at least two) spaced 1–2 minutes apart should be obtained to ensure accuracy.[81] Ambulatory blood pressure monitoring over 12 to 24 hours is the most accurate method to confirm the diagnosis.[82] An exception to this is those with very high blood pressure readings especially when there is poor organ function.[83]
With the availability of 24-hour ambulatory blood pressure monitors and home blood pressure machines, the importance of not wrongly diagnosing those who have white coat hypertension has led to a change in protocols. In the United Kingdom, current best practice is to follow up a single raised clinic reading with ambulatory measurement, or less ideally with home blood pressure monitoring over the course of 7 days.[83] The United States Preventive Services Task Force also recommends getting measurements outside of the healthcare environment.[82] Pseudohypertension in the elderly or noncompressibility artery syndrome may also require consideration. This condition is believed to be due to calcification of the arteries resulting in abnormally high blood pressure readings with a blood pressure cuff while intra arterial measurements of blood pressure are normal.[84] Orthostatic hypertension is when blood pressure increases upon standing.[85]
Other investigations
[edit]Once the diagnosis of hypertension has been made, further testing may be performed to find secondary hypertension, identify comorbidities such as diabetes, identify hypertension-caused organ damage such as chronic kidney disease or thickening of the heart muscle, and for cardiovascular disease risk stratification.[9]
Secondary hypertension is more common in preadolescent children, with most cases caused by kidney disease. Primary or essential hypertension is more common in adolescents and adults and has multiple risk factors, including obesity and a family history of hypertension.[86]
Initial assessment upon diagnosis of hypertension should include a complete history and physical examination. The World Health Organization suggests the following initial tests: serum electrolytes, serum creatinine, lipid panel, HbA1c or fasting glucose, urine dipstick and electrocardiogram (ECG/EKG).[9] Serum creatinine is measured to assess for the presence of kidney disease, which can be either the cause or the result of hypertension.[30] eGFR can also provide a baseline measurement of kidney function that can be used to monitor for side effects of certain anti-hypertensive drugs on kidney function. Testing of urine samples for protein is used as a secondary indicator of kidney disease. Lipid panel and glucose tests are done to identify comorbidities such as diabetes and hyperlipidemia and for cardiovascular risk stratification. Electrocardiogram (EKG/ECG) testing is done to check for evidence that the heart is under strain from high blood pressure, such as thickening of the heart muscle or whether the heart has experienced a prior minor disturbance such as a silent heart attack.
Classification in adults
[edit]| Categories | Systolic blood pressure, mmHg | and/or | Diastolic blood pressure, mmHg | ||
|---|---|---|---|---|---|
| Method | Office | 24h ambulatory | Office | 24h ambulatory | |
| Hypotension[87] | <110 | <100 | or | <70 | <60 |
| American College of Cardiology/American Heart Association (2017)[88] | |||||
| Normal | <120 | <115 | and | <80 | <75 |
| Elevated | 120–129 | 115–124 | and | <80 | <75 |
| Hypertension, stage 1 | 130–139 | 125–129 | or | 80–89 | 75–79 |
| Hypertension, stage 2 | ≥140 | ≥130 | or | ≥90 | ≥80 |
| European Society of Hypertension (2023)[7] | |||||
| Optimal | <120 | — | and | <80 | — |
| Normal | 120–129 | — | and/or | 80–84 | — |
| High normal | 130–139 | — | and/or | 85–89 | — |
| Hypertension, grade 1 | 140–159 | ≥130 | and/or | 90–99 | ≥80 |
| Hypertension, grade 2 | 160–179 | — | and/or | 100–109 | — |
| Hypertension, grade 3 | ≥180 | — | and/or | ≥110 | — |
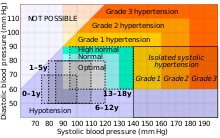
In people aged 18 years or older, hypertension is defined as either a systolic or a diastolic blood pressure measurement consistently higher than an accepted normal value (this is above 129 or 139 mmHg systolic, 89 mmHg diastolic depending on the guideline).[5][6] Lower thresholds are used if measurements are derived from 24-hour ambulatory or home monitoring.[88]
Children
[edit]Hypertension occurs in around 0.2 to 3% of newborns; however, blood pressure is not measured routinely in healthy newborns.[39] Hypertension is more common in high risk newborns. A variety of factors, such as gestational age, postconceptional age and birth weight needs to be taken into account when deciding if a blood pressure is normal in a newborn.[39]
Hypertension defined as elevated blood pressure over several visits affects 1% to 5% of children and adolescents and is associated with long-term risks of ill-health.[89] Blood pressure rises with age in childhood and, in children, hypertension is defined as an average systolic or diastolic blood pressure on three or more occasions equal or higher than the 95th percentile appropriate for the sex, age and height of the child. High blood pressure must be confirmed on repeated visits however before characterizing a child as having hypertension.[89] In adolescents, it has been proposed that hypertension is diagnosed and classified using the same criteria as in adults.[89]
Prevention
[edit]Much of the disease burden of high blood pressure is experienced by people who are not labeled as hypertensive.[90] Consequently, population strategies are required to reduce the consequences of high blood pressure and reduce the need for antihypertensive medications. Lifestyle changes are recommended to lower blood pressure.
Recommended lifestyle changes for the prevention of hypertension include:
- maintain normal body weight for adults (e.g. body mass index below 25 kg/m2)[7]
- reduce dietary sodium intake to <100 mmol/day (<6 g of salt (sodium chloride) or <2.4 g of sodium per day)[7]
- engage in regular aerobic physical activity with moderate intensity (minimum 150 minutes per week)[7]
- limit alcohol consumption,[7] max 1 drink for women and 2 for men per day[13]
- consume a diet rich in whole grains, fruit and vegetables,[7] such as the DASH diet[7]
- not smoking[7]
- stress reduction and management,[7] e.g. by meditation and yoga[7]
Effective lifestyle modification may lower blood pressure as much as an individual antihypertensive medication. Combinations of two or more lifestyle modifications can achieve even better results.[90] There is considerable evidence that reducing dietary salt intake lowers blood pressure, but whether this translates into a reduction in mortality and cardiovascular disease remains uncertain.[91] Estimated sodium intake ≥6 g/day and <3 g/day are both associated with high risk of death or major cardiovascular disease, but the association between high sodium intake and adverse outcomes is only observed in people with hypertension.[92] Consequently, in the absence of results from randomized controlled trials, the wisdom of reducing levels of dietary salt intake below 3 g/day has been questioned.[91] ESC guidelines mention periodontitis is associated with poor cardiovascular health status.[93]
The value of routine screening for hypertension is debated.[94][95][96] In 2004, the National High Blood Pressure Education Program recommended that children aged 3 years and older have blood pressure measurement at least once at every health care visit[89] and the National Heart, Lung, and Blood Institute and American Academy of Pediatrics made a similar recommendation.[97] However, the American Academy of Family Physicians[98] supports the view of the U.S. Preventive Services Task Force that the available evidence is insufficient to determine the balance of benefits and harms of screening for hypertension in children and adolescents who do not have symptoms.[99][100] The US Preventive Services Task Force recommends screening adults 18 years or older for hypertension with office blood pressure measurement.[96][101]
Management
[edit]According to one review published in 2003, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.[102]
Target blood pressure
[edit]Various expert groups have produced guidelines regarding how low the blood pressure target should be when a person is treated for hypertension. These groups recommend a target below the range 140–160 / 90–100 mmHg for the general population.[7][14][103][104] Cochrane reviews recommend similar targets for subgroups such as people with diabetes[105] and people with prior cardiovascular disease.[106] Additionally, Cochrane reviews have found that for older individuals with moderate to high cardiovascular risk, the benefits of trying to achieve a lower than standard blood pressure target (at or below 140/90 mmHg) are outweighed by the risk associated with the intervention.[107] These findings may not be applicable to other populations.[107]
Many expert groups recommend a slightly higher target of 150/90 mmHg for those over somewhere between 60 and 80 years of age.[103][104][108] The JNC 8 and American College of Physicians recommend the target of 150/90 mmHg for those over 60 years of age,[14][108] but some experts within these groups disagree with this recommendation.[109] Some expert groups have also recommended slightly lower targets in those with diabetes[110] or chronic kidney disease,[111] but others recommend the same target as for the general population.[14][105] The issue of what is the best target and whether targets should differ for high risk individuals is unresolved,[112] although some experts propose more intensive blood pressure lowering than advocated in some guidelines.[113]
For people who have never experienced cardiovascular disease who are at a 10-year risk of cardiovascular disease of less than 10%, the 2017 American Heart Association guidelines recommend medications if the systolic blood pressure is >140 mmHg or if the diastolic BP is >90 mmHg.[6] For people who have experienced cardiovascular disease or those who are at a 10-year risk of cardiovascular disease of greater than 10%, it recommends medications if the systolic blood pressure is >130 mmHg or if the diastolic BP is >80 mmHg.[6]
Lifestyle modifications
[edit]The first line of treatment for hypertension is lifestyle changes, including dietary changes, physical activity, and weight loss. Though these have all been recommended in scientific advisories,[114] a Cochrane systematic review found no evidence (due to lack of data) for effects of weight loss diets on death, long-term complications or adverse events in persons with hypertension.[115] The review did find a decrease in body weight and blood pressure.[115] Their potential effectiveness is similar to and at times exceeds a single medication.[7] If hypertension is high enough to justify immediate use of medications, lifestyle changes are still recommended in conjunction with medication.
Dietary changes shown to reduce blood pressure include diets with low sodium,[116][117] the DASH diet (Dietary Approaches to Stop Hypertension),[118] which was the best against 11 other diet in an umbrella review,[119] and plant-based diets.[120] There is some evidence green tea consumption may help lower blood pressure, but this is insufficient for it to be recommended as a treatment.[121] Hibiscus tea consumption may reduce blood pressure.[122][123] Beetroot juice consumption also may lower blood pressure.[124][125][126]
Increasing dietary potassium has a potential benefit for lowering the risk of hypertension.[127][128] The 2015 Dietary Guidelines Advisory Committee (DGAC) stated that potassium is one of the shortfall nutrients which is under-consumed in the United States.[129] However, people who take certain antihypertensive medications (such as ACE-inhibitors or ARBs) should not take potassium supplements or potassium-enriched salts due to the risk of high levels of potassium.[130]
Physical exercise regimens which are shown to reduce blood pressure include isometric resistance exercise, aerobic exercise, resistance exercise, and device-guided breathing.[131]
Stress reduction techniques such as biofeedback or transcendental meditation may be considered as an add-on to other treatments to reduce hypertension, but do not have evidence for preventing cardiovascular disease on their own.[131][132][133] Self-monitoring and appointment reminders might support the use of other strategies to improve blood pressure control, but need further evaluation.[134]
Medications
[edit]Several classes of medications, collectively referred to as antihypertensive medications, are available for treating hypertension.
First-line medications for hypertension include thiazide-diuretics, calcium channel blockers, angiotensin converting enzyme inhibitors (ACE inhibitors), and angiotensin receptor blockers (ARBs).[135][14] These medications may be used alone or in combination (ACE inhibitors and ARBs are not recommended for use together); the latter option may serve to minimize counter-regulatory mechanisms that act to restore blood pressure values to pre-treatment levels,[14][136] although the evidence for first-line combination therapy is not strong enough.[137] Most people require more than one medication to control their hypertension.[114] Medications for blood pressure control should be implemented by a stepped care approach when target levels are not reached.[134] Withdrawal of such medications in the elderly can be considered by healthcare professionals, because there is no strong evidence of an effect on mortality, myocardial infarction, or stroke.[138]
Previously, beta-blockers such as atenolol were thought to have similar beneficial effects when used as first-line therapy for hypertension. However, a Cochrane review that included 13 trials found that the effects of beta-blockers are inferior to that of other antihypertensive medications in preventing cardiovascular disease.[139]
The prescription of antihypertensive medication for children with hypertension has limited evidence. There is limited evidence which compare it with placebo and shows modest effect to blood pressure in short term. Administration of higher dose did not make the reduction of blood pressure greater.[140]
Resistant hypertension
[edit]Resistant hypertension is defined as high blood pressure that remains above a target level, in spite of being prescribed three or more antihypertensive drugs simultaneously with different mechanisms of action.[141] Failing to take prescribed medications as directed is an important cause of resistant hypertension.[142]
Some common secondary causes of resistant hypertension include obstructive sleep apnea, primary aldosteronism and renal artery stenosis, and some rare secondary causes are pheochromocytoma and coarctation of the aorta.[143] As many as one in five people with resistant hypertension have primary aldosteronism, which is a treatable and sometimes curable condition.[144] Resistant hypertension may also result from chronically high activity of the autonomic nervous system, an effect known as neurogenic hypertension.[145] Electrical therapies that stimulate the baroreflex are being studied as an option for lowering blood pressure in people in this situation.[146]
Refractory hypertension is described by one source as elevated blood pressure unmitigated by five or more concurrent antihypertensive agents of different classes.[147] People with refractory hypertension typically have increased sympathetic nervous system activity, and are at high risk for more severe cardiovascular diseases and all-cause mortality.[147][148]
Epidemiology
[edit]
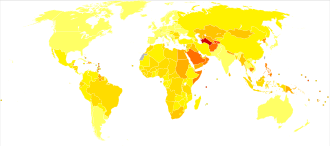
| no data <110 110–220 220–330 330–440 440–550 550–660 | 660–770 770–880 880–990 990–1100 1100–1600 >1600 |
Adults
[edit]As of 2019[update], one in three or 33% of the world population were estimated to have hypertension.[9][10] Of all people with hypertension, about 46% do not have a diagnosis of hypertension and are unaware that they have the condition.[13][9] In 1975, almost 600 million people had a diagnosis of hypertension, a number which increased to 1.13 billion by 2015 mostly due to risk factors for hypertension increasing in low- and middle-income countries.[13]
Hypertension is slightly more frequent in men.[10] In people aged under 50 years, more men than women have hypertension,[10] and in ages above 50 years the prevalence of hypertension is the same in men and women.[10] In ages above 65 years, more women than men have hypertension.[7] Hypertension becomes more common with age.[5] Hypertension is common in high, medium, and low-income countries.[13][2] It is more common in people of low socioeconomic status.[151] Hypertension is around twice as common in diabetics.[152]
In 2019, rates of diagnosed hypertension were highest in Africa (30% for both sexes), and lowest in the Americas (18% for both sexes).[10] Rates also vary markedly within regions with country-level rates as low as 22.8% (men) and 18.4% (women) in Peru and as high as 61.6% (men) and 50.9% (women) in Paraguay.[10]
In 1995 it was estimated that 24% of the United States population had hypertension or were taking antihypertensive medication.[153] By 2004 this had increased to 29%[154][155] and further to 32% (76 million US adults) by 2017.[6] In 2017, with the American guidelines' change in definition for hypertension, 46% of people in the United States are affected.[6] African-American adults in the United States have among the highest rates of hypertension in the world at 44%.[156] Differences in hypertension rates are multifactorial and under study.[157]
Children
[edit]Rates of high blood pressure in children and adolescents have increased in the last 20 years in the United States.[158] Childhood hypertension, particularly in pre-adolescents, is more often secondary to an underlying disorder than in adults. Kidney disease is the most common secondary cause of hypertension in children and adolescents. Nevertheless, primary or essential hypertension accounts for most cases.[159]
Prognosis
[edit]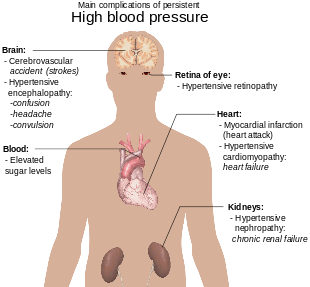
Hypertension is the most important preventable risk factor for premature death worldwide.[160] It increases the risk of ischemic heart disease,[161] stroke,[25] peripheral vascular disease,[162] and other cardiovascular diseases, including heart failure, aortic aneurysms, diffuse atherosclerosis, chronic kidney disease, atrial fibrillation, cancers, leukemia and pulmonary embolism.[12][25] Hypertension is also a risk factor for cognitive impairment and dementia.[25] Other complications include hypertensive retinopathy and hypertensive nephropathy.[30]
History
[edit]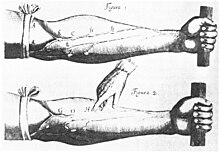
Measurement
[edit]Modern understanding of the cardiovascular system began with the work of physician William Harvey (1578–1657), who described the circulation of blood in his book "De motu cordis". The English clergyman Stephen Hales made the first published measurement of blood pressure in 1733.[163][164] However, hypertension as a clinical entity came into its own with the invention of the cuff-based sphygmomanometer by Scipione Riva-Rocci in 1896.[165] This allowed easy measurement of systolic pressure in the clinic. In 1905, Nikolai Korotkoff improved the technique by describing the Korotkoff sounds that are heard when the artery is ausculted with a stethoscope while the sphygmomanometer cuff is deflated.[164] This permitted systolic and diastolic pressure to be measured.
Identification
[edit]The symptoms similar to symptoms of patients with hypertensive crisis are discussed in medieval Persian medical texts in the chapter of "fullness disease".[166] The symptoms include headache, heaviness in the head, sluggish movements, general redness and warm to touch feel of the body, prominent, distended and tense vessels, fullness of the pulse, distension of the skin, coloured and dense urine, loss of appetite, weak eyesight, impairment of thinking, yawning, drowsiness, vascular rupture, and hemorrhagic stroke.[167] Fullness disease was presumed to be due to an excessive amount of blood within the blood vessels.
Descriptions of hypertension as a disease came among others from Thomas Young in 1808 and especially Richard Bright in 1836.[163] The first report of elevated blood pressure in a person without evidence of kidney disease was made by Frederick Akbar Mahomed (1849–1884).[168]
Until the 1990s, systolic hypertension was defined as systolic blood pressure of 160 mm Hg or greater.[169] In 1993, the WHO/ISH guidelines defined 140 mmHg as the threshold for hypertension.[170]
Treatment
[edit]Historically the treatment for what was called the "hard pulse disease" consisted in reducing the quantity of blood by bloodletting or the application of leeches.[163] This was advocated by The Yellow Emperor of China, Cornelius Celsus, Galen, and Hippocrates.[163] The therapeutic approach for the treatment of hard pulse disease included changes in lifestyle (staying away from anger and sexual intercourse) and dietary program for patients (avoiding the consumption of wine, meat, and pastries, reducing the volume of food in a meal, maintaining a low-energy diet and the dietary usage of spinach and vinegar).
In the 19th and 20th centuries, before effective pharmacological treatment for hypertension became possible, three treatment modalities were used, all with numerous side-effects: strict sodium restriction (for example the rice diet[163]), sympathectomy (surgical ablation of parts of the sympathetic nervous system), and pyrogen therapy (injection of substances that caused a fever, indirectly reducing blood pressure).[163][171]
The first chemical for hypertension, sodium thiocyanate, was used in 1900 but had many side effects and was unpopular.[163] Several other agents were developed after the Second World War, the most popular and reasonably effective of which were tetramethylammonium chloride, hexamethonium, hydralazine, and reserpine (derived from the medicinal plant Rauvolfia serpentina). None of these were well tolerated.[172][173] A major breakthrough was achieved with the discovery of the first well-tolerated orally available agents. The first was chlorothiazide, the first thiazide diuretic and developed from the antibiotic sulfanilamide, which became available in 1958.[163][174] Subsequently, beta blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers, and renin inhibitors were developed as antihypertensive agents.[171]
Society and culture
[edit]Awareness
[edit]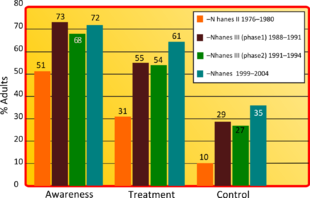
The World Health Organization has identified hypertension (high blood pressure) as the leading cause of cardiovascular mortality.[175] The World Hypertension League (WHL), an umbrella organization of 85 national hypertension societies and leagues, recognized that more than 50% of the hypertensive population worldwide are unaware of their condition.[175] To address this problem, the WHL initiated a global awareness campaign on hypertension in 2005 and dedicated 17 May of each year as World Hypertension Day.[176]
Economics
[edit]High blood pressure is the most common chronic medical problem prompting visits to primary health care providers in US. The American Heart Association estimated the direct and indirect costs of high blood pressure in 2010 as $76.6 billion.[156] In the US 80% of people with hypertension are aware of their condition, 71% take some antihypertensive medication, but only 48% of people aware that they have hypertension adequately control it.[156] Adequate management of hypertension can be hampered by inadequacies in the diagnosis, treatment, or control of high blood pressure.[177] Health care providers face many obstacles to achieving blood pressure control, including resistance to taking multiple medications to reach blood pressure goals. People also face the challenges of adhering to medicine schedules and making lifestyle changes. Nonetheless, the achievement of blood pressure goals is possible, and most importantly, lowering blood pressure significantly reduces the risk of death due to heart disease and stroke, the development of other debilitating conditions, and the cost associated with advanced medical care.[178][179]
Other animals
[edit]Hypertension in cats is indicated with a systolic blood pressure greater than 150 mmHg, with amlodipine the usual first-line treatment. A cat with a systolic blood pressure above 170 mmHg is considered hypertensive. If a cat has other problems such as any kidney disease or retina detachment then a blood pressure below 160 mmHg may also need to be monitored.[180]
Normal blood pressure in dogs can differ substantially between breeds but hypertension is often diagnosed if systolic blood pressure is above 160 mmHg particularly if this is associated with target organ damage.[181] Inhibitors of the renin-angiotensin system and calcium channel blockers are often used to treat hypertension in dogs, although other drugs may be indicated for specific conditions causing high blood pressure.[181]
See also
[edit]References
[edit]- ^ a b c d e f "About High Blood Pressure". Centers for Disease Control and Prevention (CDC). 15 May 2024. Archived from the original on 20 May 2024. Retrieved 22 May 2024.
- ^ a b c Lackland DT, Weber MA (May 2015). "Global burden of cardiovascular disease and stroke: hypertension at the core". The Canadian Journal of Cardiology. 31 (5): 569–571. doi:10.1016/j.cjca.2015.01.009. PMID 25795106.
- ^ a b Mendis S, Puska P, Norrving B (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. p. 38. ISBN 978-92-4-156437-3. Archived from the original (PDF) on 17 August 2014.
- ^ a b Hernandorena I, Duron E, Vidal JS, Hanon O (July 2017). "Treatment options and considerations for hypertensive patients to prevent dementia". Expert Opinion on Pharmacotherapy (Review). 18 (10): 989–1000. doi:10.1080/14656566.2017.1333599. PMID 28532183. S2CID 46601689.
- ^ a b c d e f g h i j k l Poulter NR, Prabhakaran D, Caulfield M (August 2015). "Hypertension". Lancet. 386 (9995): 801–812. doi:10.1016/s0140-6736(14)61468-9. PMID 25832858. S2CID 208792897.
- ^ a b c d e f g h i j Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT (June 2018). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Hypertension. 71 (6): e13–e115. doi:10.1161/HYP.0000000000000065. PMID 29133356.
- ^ a b c d e f g h i j k l m n o p q Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, et al. (1 December 2023). "2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA)". Journal of Hypertension. 41 (12): 1874–2071. doi:10.1097/HJH.0000000000003480. ISSN 1473-5598. PMID 37345492.
- ^ a b c "How Is High Blood Pressure Treated?". National Heart, Lung, and Blood Institute. 10 September 2015. Archived from the original on 6 April 2016. Retrieved 6 March 2016.
- ^ a b c d e f g h i j k Global report on hypertension: the race against a silent killer. Geneva: World Health Organization (WHO). 19 September 2023. ISBN 978-92-4-008106-2.
- ^ a b c d e f g Ezzati M, Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, et al. (NCD Risk Factor Collaboration) (11 September 2021). "Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants". The Lancet. 398 (10304): 957–980. doi:10.1016/S0140-6736(21)01330-1. ISSN 0140-6736. PMC 8446938. PMID 34450083. S2CID 237286310.
- ^ a b Naish J, Court DS (2014). Medical sciences (2 ed.). Elsevier Health Sciences. p. 562. ISBN 978-0-7020-5249-1.
- ^ a b Lau DH, Nattel S, Kalman JM, Sanders P (August 2017). "Modifiable Risk Factors and Atrial Fibrillation". Circulation (Review). 136 (6): 583–596. doi:10.1161/CIRCULATIONAHA.116.023163. PMID 28784826.
- ^ a b c d e f "Hypertension". World Health Organization (WHO). 16 March 2023. Retrieved 22 May 2024.
- ^ a b c d e f James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Narva AS, Ortiz E (February 2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–520. doi:10.1001/jama.2013.284427. PMID 24352797.
- ^ Musini VM, Tejani AM, Bassett K, Puil L, Wright JM (June 2019). "Pharmacotherapy for hypertension in adults 60 years or older". The Cochrane Database of Systematic Reviews. 6 (6): CD000028. doi:10.1002/14651858.CD000028.pub3. PMC 6550717. PMID 31167038.
- ^ Sundström J, Arima H, Jackson R, Turnbull F, Rahimi K, Chalmers J, Woodward M, Neal B (February 2015). "Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis". Annals of Internal Medicine. 162 (3): 184–191. doi:10.7326/M14-0773. PMID 25531552. S2CID 46553658.
- ^ Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, Chalmers J, Mant J, Salam A, Rahimi K, Perkovic V, Rodgers A (January 2016). "Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis". Lancet. 387 (10017): 435–443. doi:10.1016/S0140-6736(15)00805-3. PMID 26559744. S2CID 36805676. Archived from the original on 16 April 2019. Retrieved 11 February 2019.
- ^ Diao D, Wright JM, Cundiff DK, Gueyffier F (August 2012). "Pharmacotherapy for mild hypertension". The Cochrane Database of Systematic Reviews. 8 (8): CD006742. doi:10.1002/14651858.CD006742.pub2. PMC 8985074. PMID 22895954. S2CID 42363250.
- ^ Garrison SR, Kolber MR, Korownyk CS, McCracken RK, Heran BS, Allan GM (August 2017). "Blood pressure targets for hypertension in older adults". The Cochrane Database of Systematic Reviews. 2017 (8): CD011575. doi:10.1002/14651858.CD011575.pub2. PMC 6483478. PMID 28787537.
- ^ Musini VM, Gueyffier F, Puil L, Salzwedel DM, Wright JM (August 2017). "Pharmacotherapy for hypertension in adults aged 18 to 59 years". The Cochrane Database of Systematic Reviews. 2017 (8): CD008276. doi:10.1002/14651858.CD008276.pub2. PMC 6483466. PMID 28813123.
- ^ a b Fisher ND, Williams GH (2005). "Hypertensive vascular disease". In Kasper DL, Braunwald E, Fauci AS, et al. (eds.). Harrison's Principles of Internal Medicine (16th ed.). New York: McGraw-Hill. pp. 1463–1481. ISBN 978-0-07-139140-5.
- ^ Marshall IJ, Wolfe CD, McKevitt C (July 2012). "Lay perspectives on hypertension and drug adherence: systematic review of qualitative research". The BMJ. 345: e3953. doi:10.1136/bmj.e3953. PMC 3392078. PMID 22777025.
- ^ Wong TY, Wong T, Mitchell P (February 2007). "The eye in hypertension". Lancet. 369 (9559): 425–435. doi:10.1016/S0140-6736(07)60198-6. PMID 17276782. S2CID 28579025.
- ^ "Truncal obesity (Concept Id: C4551560) – MedGen – NCBI". ncbi.nlm.nih.gov. Retrieved 24 April 2022.
- ^ a b c d e f g h i j k l m O'Brien E, Beevers DG, Lip GY (2007). ABC of hypertension. London: BMJ Books. ISBN 978-1-4051-3061-5.
- ^ "High Blood Pressure – Understanding the Silent Killer". Center for Drug Evaluation and Research. U.S. Food and Drug Administration. 21 January 2021.
- ^ Rodriguez MA, Kumar SK, De Caro M (1 April 2010). "Hypertensive crisis". Cardiology in Review. 18 (2): 102–107. doi:10.1097/CRD.0b013e3181c307b7. PMID 20160537. S2CID 34137590.
- ^ "Hypertensive Crisis". heart.org. Archived from the original on 25 July 2015. Retrieved 25 July 2015.
- ^ a b c Marik PE, Varon J (June 2007). "Hypertensive crises: challenges and management". Chest. 131 (6): 1949–1962. doi:10.1378/chest.06-2490. PMID 17565029. Archived from the original on 4 December 2012.
- ^ a b c Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, et al. (Joint National Committee on Prevention, National High Blood Pressure Education Program Coordinating Committee) (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension. 42 (6): 1206–1252. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
- ^ a b Perez MI, Musini VM (January 2008). "Pharmacological interventions for hypertensive emergencies". The Cochrane Database of Systematic Reviews. 2008 (1): CD003653. doi:10.1002/14651858.CD003653.pub3. PMC 6991936. PMID 18254026.
- ^ Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill. 2011. pp. 55–61. ISBN 978-0-07-174889-6.
- ^ a b "Management of hypertension in pregnant and postpartum women". uptodate.com. Archived from the original on 4 March 2016. Retrieved 30 July 2015.
- ^ Al Khalaf SY, O'Reilly ÉJ, Barrett PM, B Leite DF, Pawley LC, McCarthy FP, Khashan AS (May 2021). "Impact of Chronic Hypertension and Antihypertensive Treatment on Adverse Perinatal Outcomes: Systematic Review and Meta-Analysis". Journal of the American Heart Association. 10 (9): e018494. doi:10.1161/JAHA.120.018494. PMC 8200761. PMID 33870708.
- ^ "Pregnancy complications increase the risk of heart attacks and stroke in women with high blood pressure". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 21 November 2023. doi:10.3310/nihrevidence_60660. S2CID 265356623.
- ^ Al Khalaf S, Chappell LC, Khashan AS, McCarthy FP, O'Reilly ÉJ (July 2023). "Association Between Chronic Hypertension and the Risk of 12 Cardiovascular Diseases Among Parous Women: The Role of Adverse Pregnancy Outcomes". Hypertension. 80 (7): 1427–1438. doi:10.1161/HYPERTENSIONAHA.122.20628. PMID 37170819.
- ^ Gibson P (30 July 2009). "Hypertension and Pregnancy". eMedicine Obstetrics and Gynecology. Medscape. Archived from the original on 24 July 2009. Retrieved 16 June 2009.
- ^ a b Rodriguez-Cruz E, Ettinger LM (6 April 2010). "Hypertension". eMedicine Pediatrics: Cardiac Disease and Critical Care Medicine. Medscape. Archived from the original on 15 August 2009. Retrieved 16 June 2009.
- ^ a b c Dionne JM, Abitbol CL, Flynn JT (January 2012). "Hypertension in infancy: diagnosis, management and outcome". Pediatric Nephrology. 27 (1): 17–32. doi:10.1007/s00467-010-1755-z. PMID 21258818. S2CID 10698052.
- ^ Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, Chasman DI, et al. (September 2011). "Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk". Nature. 478 (7367): 103–109. Bibcode:2011Natur.478..103T. doi:10.1038/nature10405. PMC 3340926. PMID 21909115.
- ^ Lifton RP, Gharavi AG, Geller DS (February 2001). "Molecular mechanisms of human hypertension". Cell. 104 (4): 545–556. doi:10.1016/S0092-8674(01)00241-0. PMID 11239411.
- ^ a b Kato N, Loh M, Takeuchi F, Verweij N, Wang X, Zhang W, et al. (November 2015). "Trans-ancestry genome-wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation". Nature Genetics. 47 (11): 1282–1293. doi:10.1038/ng.3405. PMC 4719169. PMID 26390057.
- ^ Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D'Agostino RB, Levy D (February 2002). "Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study". JAMA. 287 (8): 1003–1010. doi:10.1001/jama.287.8.1003. PMID 11866648.
- ^ Carrera-Bastos P, Fontes-Villalba M, O'Keefe JH, Lindeberg S, Cordain L (9 March 2011). "The western diet and lifestyle and diseases of civilization". Research Reports in Clinical Cardiology. 2: 15–35. doi:10.2147/RRCC.S16919. S2CID 3231706. Retrieved 9 February 2021.
- ^ Mesas AE, Leon-Muñoz LM, Rodriguez-Artalejo F, Lopez-Garcia E (October 2011). "The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis". The American Journal of Clinical Nutrition. 94 (4): 1113–1126. doi:10.3945/ajcn.111.016667. PMID 21880846.
- ^ Vaidya A, Forman JP (November 2010). "Vitamin D and hypertension: current evidence and future directions". Hypertension. 56 (5): 774–779. doi:10.1161/HYPERTENSIONAHA.109.140160. PMID 20937970.
- ^ Sorof J, Daniels S (October 2002). "Obesity hypertension in children: a problem of epidemic proportions". Hypertension. 40 (4): 441–447. doi:10.1161/01.HYP.0000032940.33466.12. PMID 12364344.
- ^ Lawlor DA, Smith GD (May 2005). "Early life determinants of adult blood pressure". Current Opinion in Nephrology and Hypertension. 14 (3): 259–264. doi:10.1097/01.mnh.0000165893.13620.2b. PMID 15821420. S2CID 10646150.
- ^ Gois PH, Souza ER (September 2020). "Pharmacotherapy for hyperuricaemia in hypertensive patients". The Cochrane Database of Systematic Reviews. 2020 (9): CD008652. doi:10.1002/14651858.CD008652.pub4. PMC 8094453. PMID 32877573.
- ^ Fares A (June 2013). "Winter Hypertension: Potential mechanisms". International Journal of Health Sciences. 7 (2): 210–219. doi:10.12816/0006044. PMC 3883610. PMID 24421749.
- ^ Muñoz Aguilera E, Suvan J, Buti J, Czesnikiewicz-Guzik M, Barbosa Ribeiro A, Orlandi M, et al. (January 2020). Lembo G (ed.). "Periodontitis is associated with hypertension: a systematic review and meta-analysis". Cardiovascular Research. 116 (1): 28–39. doi:10.1093/cvr/cvz201. PMID 31549149.
- ^ Dluhy RG, Williams GH (1998). "Endocrine hypertension". In Wilson JD, Foster DW, Kronenberg HM (eds.). Williams textbook of endocrinology (9th ed.). Philadelphia; Montreal: W.B. Saunders. pp. 729–749. ISBN 978-0-7216-6152-0.
- ^ Grossman E, Messerli FH (January 2012). "Drug-induced hypertension: an unappreciated cause of secondary hypertension". The American Journal of Medicine. 125 (1): 14–22. doi:10.1016/j.amjmed.2011.05.024. PMID 22195528.
- ^ Jiang J, Liu M, Parvez F, Wang B, Wu F, Eunus M, Bangalore S, Newman JD, Ahmed A, Islam T, Rakibuz-Zaman M, Hasan R, Sarwar G, Levy D, Slavkovich V, Argos M, Scannell Bryan M, Farzan SF, Hayes RB, Graziano JH, Ahsan H, Chen Y (August 2015). "Association between Arsenic Exposure from Drinking Water and Longitudinal Change in Blood Pressure among HEALS Cohort Participants". Environmental Health Perspectives. 123 (8): 806–812. doi:10.1289/ehp.1409004. PMC 4529016. PMID 25816368.
- ^ Abhyankar LN, Jones MR, Guallar E, Navas-Acien A (April 2012). "Arsenic exposure and hypertension: a systematic review". Environmental Health Perspectives. 120 (4): 494–500. doi:10.1289/ehp.1103988. PMC 3339454. PMID 22138666.
- ^ Meng L, Chen D, Yang Y, Zheng Y, Hui R (May 2012). "Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies". Journal of Hypertension. 30 (5): 842–851. doi:10.1097/hjh.0b013e32835080b7. PMID 22343537. S2CID 32187480.
- ^ Hawkley LC, Cacioppo JT (October 2010). "Loneliness matters: a theoretical and empirical review of consequences and mechanisms". Annals of Behavioral Medicine. 40 (2): 218–227. doi:10.1007/s12160-010-9210-8. PMC 3874845. PMID 20652462.
- ^ Yang BY, Qian Z, Howard SW, Vaughn MG, Fan SJ, Liu KK, Dong GH (April 2018). "Global association between ambient air pollution and blood pressure: A systematic review and meta-analysis". Environmental Pollution. 235: 576–588. Bibcode:2018EPoll.235..576Y. doi:10.1016/j.envpol.2018.01.001. PMID 29331891.
- ^ Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OS, Krishnan RJ, Raifu AO, Rehm J (June 2018). "Sex-Specific Associations Between Alcohol Consumption and Incidence of Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies". Journal of the American Heart Association. 7 (13): e008202. doi:10.1161/JAHA.117.008202. PMC 6064910. PMID 29950485.
- ^ Conway J (April 1984). "Hemodynamic aspects of essential hypertension in humans". Physiological Reviews. 64 (2): 617–660. doi:10.1152/physrev.1984.64.2.617. PMID 6369352.
- ^ a b Palatini P, Julius S (June 2009). "The role of cardiac autonomic function in hypertension and cardiovascular disease". Current Hypertension Reports. 11 (3): 199–205. doi:10.1007/s11906-009-0035-4. PMID 19442329. S2CID 11320300.
- ^ Andersson OK, Lingman M, Himmelmann A, Sivertsson R, Widgren BR (2004). "Prediction of future hypertension by casual blood pressure or invasive hemodynamics? A 30-year follow-up study". Blood Pressure. 13 (6): 350–354. doi:10.1080/08037050410004819. PMID 15771219. S2CID 28992820.
- ^ Folkow B (April 1982). "Physiological aspects of primary hypertension". Physiological Reviews. 62 (2): 347–504. doi:10.1152/physrev.1982.62.2.347. PMID 6461865.
- ^ Struijker Boudier HA, le Noble JL, Messing MW, Huijberts MS, le Noble FA, van Essen H (December 1992). "The microcirculation and hypertension". Journal of Hypertension Supplement. 10 (7): S147–156. doi:10.1097/00004872-199212000-00016. PMID 1291649.
- ^ Schiffrin EL (February 1992). "Reactivity of small blood vessels in hypertension: relation with structural changes. State of the art lecture". Hypertension. 19 (2 Suppl): II1-9. doi:10.1161/01.HYP.19.2_Suppl.II1-a. PMID 1735561.
- ^ Safar ME, London GM (August 1987). "Arterial and venous compliance in sustained essential hypertension". Hypertension. 10 (2): 133–139. doi:10.1161/01.HYP.10.2.133. PMID 3301662.
- ^ Kim SH, Lim KR, Chun KJ (2022). "Higher heart rate variability as a predictor of atrial fibrillation in patients with hypertensione". Scientific Reports. 12 (1): 3702. Bibcode:2022NatSR..12.3702K. doi:10.1038/s41598-022-07783-3. PMC 8904557. PMID 35260686.
- ^ Steppan J, Barodka V, Berkowitz DE, Nyhan D (2 August 2011). "Vascular stiffness and increased pulse pressure in the aging cardiovascular system". Cardiology Research and Practice. 2011: 263585. doi:10.4061/2011/263585. PMC 3154449. PMID 21845218.
- ^ Chobanian AV (August 2007). "Clinical practice. Isolated systolic hypertension in the elderly". The New England Journal of Medicine. 357 (8): 789–796. doi:10.1056/NEJMcp071137. PMID 17715411. S2CID 42515260.
- ^ Zieman SJ, Melenovsky V, Kass DA (May 2005). "Mechanisms, pathophysiology, and therapy of arterial stiffness". Arteriosclerosis, Thrombosis, and Vascular Biology. 25 (5): 932–943. doi:10.1161/01.ATV.0000160548.78317.29. PMID 15731494.
- ^ Navar LG (December 2010). "Counterpoint: Activation of the intrarenal renin-angiotensin system is the dominant contributor to systemic hypertension". Journal of Applied Physiology. 109 (6): 1998–2000, discussion 2015. doi:10.1152/japplphysiol.00182.2010a. PMC 3006411. PMID 21148349.
- ^ Esler M, Lambert E, Schlaich M (December 2010). "Point: Chronic activation of the sympathetic nervous system is the dominant contributor to systemic hypertension". Journal of Applied Physiology. 109 (6): 1996–1998, discussion 2016. doi:10.1152/japplphysiol.00182.2010. PMID 20185633. S2CID 7685157.
- ^ Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S (June 2009). "Endothelium-dependent contractions and endothelial dysfunction in human hypertension". British Journal of Pharmacology. 157 (4): 527–536. doi:10.1111/j.1476-5381.2009.00240.x. PMC 2707964. PMID 19630832.
- ^ Marchesi C, Paradis P, Schiffrin EL (July 2008). "Role of the renin-angiotensin system in vascular inflammation". Trends in Pharmacological Sciences. 29 (7): 367–374. doi:10.1016/j.tips.2008.05.003. PMID 18579222.
- ^ Gooch JL, Sharma AC (September 2014). "Targeting the immune system to treat hypertension: where are we?". Current Opinion in Nephrology and Hypertension. 23 (5): 473–479. doi:10.1097/MNH.0000000000000052. PMID 25036747. S2CID 13383731.
- ^ Adrogué HJ, Madias NE (May 2007). "Sodium and potassium in the pathogenesis of hypertension". The New England Journal of Medicine. 356 (19): 1966–1978. doi:10.1056/NEJMra064486. PMID 17494929. S2CID 22345731.
- ^ Perez V, Chang ET (November 2014). "Sodium-to-potassium ratio and blood pressure, hypertension, and related factors". Advances in Nutrition. 5 (6): 712–741. doi:10.3945/an.114.006783. PMC 4224208. PMID 25398734.
- ^ Williams GH, Hollenberg NK (November 1985). "Non-modulating essential hypertension: a subset particularly responsive to converting enzyme inhibitors". Journal of Hypertension Supplement. 3 (2): S81–S87. PMID 3003304.
- ^ Harrison TR, Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. (2018). Harrison's Principles of Internal Medicine (20th ed.). McGraw-Hill Education. p. 1896. ISBN 978-1-259-64404-7.
When plasma renin activity (PRA) is plotted against 24-h sodium excretion, ~10–15% of hypertensive patients have high PRA and 25% have low PRA. High-renin patients may have a vasoconstrictor form of hypertension, whereas low-renin patients may have volume-dependent hypertension.
- ^ a b c d e f g h Viera AJ (July 2017). "Screening for Hypertension and Lowering Blood Pressure for Prevention of Cardiovascular Disease Events". The Medical Clinics of North America (Review). 101 (4): 701–712. doi:10.1016/j.mcna.2017.03.003. PMID 28577621.
- ^ a b c Vischer AS, Burkard T (2017). "Principles of Blood Pressure Measurement – Current Techniques, Office vs Ambulatory Blood Pressure Measurement". Hypertension: From basic research to clinical practice (Review). Advances in Experimental Medicine and Biology. Vol. 956. pp. 85–96. doi:10.1007/5584_2016_49. ISBN 978-3-319-44250-1. PMID 27417699.
- ^ a b Siu AL (November 2015). "Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 163 (10): 778–786. doi:10.7326/m15-2223. PMID 26458123.
- ^ a b National Clinical Guidance Centre (August 2011). "7 Diagnosis of Hypertension, 7.5 Link from evidence to recommendations" (PDF). Hypertension (NICE CG 127). National Institute for Health and Clinical Excellence. p. 102. Archived from the original (PDF) on 23 July 2013. Retrieved 22 December 2011.
- ^ Franklin SS, Wilkinson IB, McEniery CM (February 2012). "Unusual hypertensive phenotypes: what is their significance?". Hypertension. 59 (2): 173–178. doi:10.1161/HYPERTENSIONAHA.111.182956. PMID 22184330.
- ^ Kario K (June 2009). "Orthostatic hypertension: a measure of blood pressure variation for predicting cardiovascular risk". Circulation Journal. 73 (6): 1002–1007. doi:10.1253/circj.cj-09-0286. PMID 19430163.
- ^ Luma GB, Spiotta RT (May 2006). "Hypertension in children and adolescents". American Family Physician. 73 (9): 1558–1568. PMID 16719248.
- ^ Divisón-Garrote JA, Banegas JR, De la Cruz JJ, Escobar-Cervantes C, De la Sierra A, Gorostidi M, Vinyoles E, Abellán-Aleman J, Segura J, Ruilope LM (1 September 2016). "Hypotension based on office and ambulatory monitoring blood pressure. Prevalence and clinical profile among a cohort of 70,997 treated hypertensives". Journal of the American Society of Hypertension: JASH. 10 (9): 714–723. doi:10.1016/j.jash.2016.06.035. ISSN 1878-7436. PMID 27451950.
- ^ a b Whelton PK, Carey RM, Mancia G, Kreutz R, Bundy JD, Williams B (14 September 2022). "Harmonization of the American College of Cardiology/American Heart Association and European Society of Cardiology/European Society of Hypertension Blood Pressure/Hypertension Guidelines". European Heart Journal. 43 (35): 3302–3311. doi:10.1093/eurheartj/ehac432. ISSN 0195-668X. PMC 9470378. PMID 36100239.
- ^ a b c d National High Blood Pressure Education Program Working Group on High Blood Pressure in Children Adolescents (August 2004). "The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents". Pediatrics. 114 (2 Suppl 4th Report): 555–576. doi:10.1542/peds.114.2.S2.555. hdl:2027/uc1.c095473177. PMID 15286277.
- ^ a b Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, Sever PS, McG Thom S (March 2004). "Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV". Journal of Human Hypertension. 18 (3): 139–185. doi:10.1038/sj.jhh.1001683. PMID 14973512.
- ^ a b "Evidence-based policy for salt reduction is needed". Lancet. 388 (10043): 438. July 2016. doi:10.1016/S0140-6736(16)31205-3. PMID 27507743. S2CID 205982690.
- ^ Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Li W, Lu Y, Yi S, Rensheng L, Iqbal R, Mony P, Yusuf R, Yusoff K, Szuba A, Oguz A, Rosengren A, Bahonar A, Yusufali A, Schutte AE, Chifamba J, Mann JF, Anand SS, Teo K, Yusuf S (July 2016). "Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies". Lancet. 388 (10043): 464–475. doi:10.1016/S0140-6736(16)30467-6. hdl:10379/16625. PMID 27216139. S2CID 44581906.
The results showed that cardiovascular disease and death are increased with low sodium intake (compared with moderate intake) irrespective of hypertension status, whereas there is a higher risk of cardiovascular disease and death only in individuals with hypertension consuming more than 6 g of sodium per day (representing only 10% of the population studied)
- ^ Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvänne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F (July 2012). "European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts)". European Heart Journal. 33 (13): 1635–1701. doi:10.1093/eurheartj/ehs092. PMID 22555213.
- ^ Chiolero A, Bovet P, Paradis G (March 2013). "Screening for elevated blood pressure in children and adolescents: a critical appraisal". JAMA Pediatrics. 167 (3): 266–273. doi:10.1001/jamapediatrics.2013.438. PMID 23303490.
- ^ Daniels SR, Gidding SS (March 2013). "Blood pressure screening in children and adolescents: is the glass half empty or more than half full?". JAMA Pediatrics. 167 (3): 302–304. doi:10.1001/jamapediatrics.2013.439. PMID 23303514.
- ^ a b Schmidt BM, Durao S, Toews I, Bavuma CM, Hohlfeld A, Nury E, et al. (Cochrane Hypertension Group) (May 2020). "Screening strategies for hypertension". The Cochrane Database of Systematic Reviews. 2020 (5): CD013212. doi:10.1002/14651858.CD013212.pub2. PMC 7203601. PMID 32378196.
- ^ "Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report". Pediatrics. 128 (Suppl 5): S213–S256. December 2011. doi:10.1542/peds.2009-2107C. PMC 4536582. PMID 22084329.
- ^ "Hypertension – Clinical Preventive Service Recommendation". Archived from the original on 1 November 2014. Retrieved 13 October 2013.
- ^ Moyer VA (November 2013). "Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 159 (9): 613–619. doi:10.7326/0003-4819-159-9-201311050-00725. PMID 24097285. S2CID 20193715.
- ^ "Document | United States Preventive Services Taskforce". uspreventiveservicestaskforce.org. Archived from the original on 22 May 2020. Retrieved 22 April 2020.
- ^ Krist AH, Davidson KW, Mangione CM, Cabana M, Caughey AB, Davis EM, et al. (April 2021). "Screening for Hypertension in Adults: US Preventive Services Task Force Reaffirmation Recommendation Statement". JAMA. 325 (16): 1650–1656. doi:10.1001/jama.2021.4987. PMID 33904861. S2CID 233409679.
- ^ Law M, Wald N, Morris J (2003). "Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy". Health Technology Assessment. 7 (31): 1–94. doi:10.3310/hta7310. PMID 14604498.
- ^ a b Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. (May 2015). "The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension". The Canadian Journal of Cardiology. 31 (5): 549–568. doi:10.1016/j.cjca.2015.02.016. PMID 25936483.
- ^ a b "Hypertension: Recommendations, Guidance and guidelines". NICE. Archived from the original on 3 October 2006. Retrieved 4 August 2015.
- ^ a b Arguedas JA, Leiva V, Wright JM (October 2013). "Blood pressure targets for hypertension in people with diabetes mellitus". The Cochrane Database of Systematic Reviews (10): CD008277. doi:10.1002/14651858.cd008277.pub2. PMID 24170669.
- ^ Saiz LC, Gorricho J, Garjón J, Celaya MC, Erviti J, Leache L (November 2022). "Blood pressure targets for the treatment of people with hypertension and cardiovascular disease". The Cochrane Database of Systematic Reviews. 2022 (11): CD010315. doi:10.1002/14651858.CD010315.pub5. PMC 9673465. PMID 36398903.
- ^ a b Arguedas JA, Leiva V, Wright JM (December 2020). "Blood pressure targets in adults with hypertension". The Cochrane Database of Systematic Reviews. 2020 (12): CD004349. doi:10.1002/14651858.CD004349.pub3. PMC 8094587. PMID 33332584.
- ^ a b Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA (March 2017). "Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians". Annals of Internal Medicine. 166 (6): 430–437. doi:10.7326/M16-1785. PMID 28135725.
- ^ Wright JT, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR (April 2014). "Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view". Annals of Internal Medicine. 160 (7): 499–503. doi:10.7326/m13-2981. PMID 24424788.
- ^ Passarella P, Kiseleva TA, Valeeva FV, Gosmanov AR (1 August 2018). "Hypertension Management in Diabetes: 2018 Update". Diabetes Spectrum. 31 (3): 218–224. doi:10.2337/ds17-0085. ISSN 1040-9165. PMC 6092891. PMID 30140137.
- ^ Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH, Knoll GA, Muntner P, Pecoits-Filho R, Sarnak MJ, Tobe SW, Tomson CR, Mann JF (March 2021). "KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease". Kidney International. 99 (3): S1–S87. doi:10.1016/j.kint.2020.11.003. PMID 33637192.
- ^ Brunström M, Carlberg B (January 2016). "Lower blood pressure targets: to whom do they apply?". Lancet. 387 (10017): 405–406. doi:10.1016/S0140-6736(15)00816-8. PMID 26559745. S2CID 44282689.
- ^ Xie X, Atkins E, Lv J, Rodgers A (June 2016). "Intensive blood pressure lowering – Authors' reply". Lancet. 387 (10035): 2291. doi:10.1016/S0140-6736(16)30366-X. PMID 27302266.
- ^ a b Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, Sanchez E (April 2014). "An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention". Hypertension. 63 (4): 878–885. doi:10.1161/HYP.0000000000000003. PMC 10280688. PMID 24243703.
- ^ a b Semlitsch T, Krenn C, Jeitler K, Berghold A, Horvath K, Siebenhofer A (February 2021). "Long-term effects of weight-reducing diets in people with hypertension". The Cochrane Database of Systematic Reviews. 2021 (2): CD008274. doi:10.1002/14651858.CD008274.pub4. PMC 8093137. PMID 33555049.
- ^ He FJ, Li J, Macgregor GA (April 2013). "Effect of longer-term modest salt reduction on blood pressure". The Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 30 (4): CD004937. doi:10.1002/14651858.CD004937.pub2. PMID 23633321. S2CID 23522004.
- ^ Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NR, et al. (February 2020). "Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials". The BMJ. 368: m315. doi:10.1136/bmj.m315. PMC 7190039. PMID 32094151.
- ^ Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. (January 2001). "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group". The New England Journal of Medicine. 344 (1): 3–10. doi:10.1056/NEJM200101043440101. PMID 11136953.
- ^ Sukhato K, Akksilp K, Dellow A, Vathesatogkit P, Anothaisintawee T (December 2020). "Efficacy of different dietary patterns on lowering of blood pressure level: an umbrella review". The American Journal of Clinical Nutrition. 112 (6): 1584–1598. doi:10.1093/ajcn/nqaa252. PMID 33022695.
- ^ Joshi S, Ettinger L, Liebman SE (2020). "Plant-Based Diets and Hypertension". American Journal of Lifestyle Medicine. 14 (4): 397–405. doi:10.1177/1559827619875411. PMC 7692016. PMID 33281520.
- ^ Xu R, Yang K, Ding J, Chen G (February 2020). "Effect of green tea supplementation on blood pressure: A systematic review and meta-analysis of randomized controlled trials". Medicine. 99 (6): e19047. doi:10.1097/MD.0000000000019047. PMC 7015560. PMID 32028419.
- ^ Najafpour Boushehri S, Karimbeiki R, Ghasempour S, Ghalishourani SS, Pourmasoumi M, Hadi A, et al. (February 2020). "The efficacy of sour tea (Hibiscus sabdariffa L.) on selected cardiovascular disease risk factors: A systematic review and meta-analysis of randomized clinical trials". Phytotherapy Research. 34 (2): 329–339. doi:10.1002/ptr.6541. PMID 31943427. S2CID 210333560.
- ^ McKay DL, Chen CY, Saltzman E, Blumberg JB (February 2010). "Hibiscus sabdariffa L. tea (tisane) lowers blood pressure in prehypertensive and mildly hypertensive adults". The Journal of Nutrition. 140 (2): 298–303. doi:10.3945/jn.109.115097. PMID 20018807.
- ^ "Beetroot juice lowers high blood pressure, suggests research". British Heart Foundation.
- ^ Siervo M, Lara J, Ogbonmwan I, Mathers JC (June 2013). "Inorganic nitrate and beetroot juice supplementation reduces blood pressure in adults: a systematic review and meta-analysis". The Journal of Nutrition. 143 (6): 818–826. doi:10.3945/jn.112.170233. PMID 23596162.
- ^ Bahadoran Z, Mirmiran P, Kabir A, Azizi F, Ghasemi A (November 2017). "The Nitrate-Independent Blood Pressure-Lowering Effect of Beetroot Juice: A Systematic Review and Meta-Analysis". Advances in Nutrition. 8 (6): 830–838. doi:10.3945/an.117.016717. PMC 5683004. PMID 29141968.
- ^ Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP (April 2013). "Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses". The BMJ. 346: f1378. doi:10.1136/bmj.f1378. PMC 4816263. PMID 23558164.
- ^ Stone MS, Martyn L, Weaver CM (July 2016). "Potassium Intake, Bioavailability, Hypertension, and Glucose Control". Nutrients. 8 (7): 444. doi:10.3390/nu8070444. PMC 4963920. PMID 27455317.
- ^ "Scientific Report of the 2015 Dietary Guidelines Advisory Committee". Archived from the original on 26 April 2017. Retrieved 26 April 2017.
- ^ Raebel MA (June 2012). "Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers". Cardiovascular Therapeutics. 30 (3): e156–166. doi:10.1111/j.1755-5922.2010.00258.x. PMID 21883995.
- ^ a b Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, Fuchs FD, Hughes JW, Lackland DT, Staffileno BA, Townsend RR, Rajagopalan S (June 2013). "Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association". Hypertension. 61 (6): 1360–1383. doi:10.1161/HYP.0b013e318293645f. PMID 23608661.
- ^ Nagele E, Jeitler K, Horvath K, Semlitsch T, Posch N, Herrmann KH, Grouven U, Hermanns T, Hemkens LG, Siebenhofer A (October 2014). "Clinical effectiveness of stress-reduction techniques in patients with hypertension: systematic review and meta-analysis". Journal of Hypertension. 32 (10): 1936–1944, discussion 1944. doi:10.1097/HJH.0000000000000298. PMID 25084308. S2CID 20098894.
- ^ Dickinson HO, Campbell F, Beyer FR, Nicolson DJ, Cook JV, Ford GA, Mason JM (January 2008). "Relaxation therapies for the management of primary hypertension in adults". The Cochrane Database of Systematic Reviews (1): CD004935. doi:10.1002/14651858.CD004935.pub2. PMID 18254065.
- ^ a b Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T (March 2010). "Interventions used to improve control of blood pressure in patients with hypertension" (PDF). The Cochrane Database of Systematic Reviews (3): CD005182. doi:10.1002/14651858.cd005182.pub4. hdl:10344/9179. PMID 20238338. Archived (PDF) from the original on 12 April 2019. Retrieved 11 February 2019.
- ^ Wright JM, Musini VM, Gill R (April 2018). "First-line drugs for hypertension". The Cochrane Database of Systematic Reviews. 2018 (4): CD001841. doi:10.1002/14651858.CD001841.pub3. PMC 6513559. PMID 29667175.
- ^ Chen JM, Heran BS, Wright JM (October 2009). "Blood pressure lowering efficacy of diuretics as second-line therapy for primary hypertension". The Cochrane Database of Systematic Reviews (4): CD007187. doi:10.1002/14651858.CD007187.pub2. PMID 19821398. S2CID 73993182.
- ^ Garjón J, Saiz LC, Azparren A, Gaminde I, Ariz MJ, Erviti J, et al. (Cochrane Hypertension Group) (February 2020). "First-line combination therapy versus first-line monotherapy for primary hypertension". The Cochrane Database of Systematic Reviews. 2 (2): CD010316. doi:10.1002/14651858.CD010316.pub3. PMC 7002970. PMID 32026465.
- ^ Reeve E, Jordan V, Thompson W, Sawan M, Todd A, Gammie TM, et al. (Cochrane Hypertension Group) (June 2020). "Withdrawal of antihypertensive drugs in older people". The Cochrane Database of Systematic Reviews. 2020 (6): CD012572. doi:10.1002/14651858.CD012572.pub2. PMC 7387859. PMID 32519776.
- ^ Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH (January 2017). "Beta-blockers for hypertension". The Cochrane Database of Systematic Reviews. 1 (1): CD002003. doi:10.1002/14651858.CD002003.pub5. PMC 5369873. PMID 28107561.
- ^ Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh R, et al. (Cochrane Hypertension Group) (February 2014). "Pharmacological interventions for hypertension in children". The Cochrane Database of Systematic Reviews (2): CD008117. doi:10.1002/14651858.CD008117.pub2. PMC 11056235. PMID 24488616.
- ^ Giacona JM, Kositanurit W, Vongpatanasin W (April 2024). "Management of Resistant Hypertension-An Update". JAMA Intern Med. 184 (4): 433–434. doi:10.1001/jamainternmed.2023.8555. PMID 38372970.
- ^ Santschi V, Chiolero A, Burnier M (November 2009). "Electronic monitors of drug adherence: tools to make rational therapeutic decisions". Journal of Hypertension. 27 (11): 2294–2295, author reply 2295. doi:10.1097/hjh.0b013e328332a501. PMID 20724871.
- ^ Sarwar MS, Islam MS, Al Baker SM, Hasnat A (May 2013). "Resistant hypertension: underlying causes and treatment". Drug Research. 63 (5): 217–223. doi:10.1055/s-0033-1337930. PMID 23526242. S2CID 8247941.
- ^ Young WF (February 2019). "Diagnosis and treatment of primary aldosteronism: practical clinical perspectives". Journal of Internal Medicine. 285 (2): 126–148. doi:10.1111/joim.12831. PMID 30255616. S2CID 52824356.
- ^ Zubcevic J, Waki H, Raizada MK, Paton JF (June 2011). "Autonomic-immune-vascular interaction: an emerging concept for neurogenic hypertension". Hypertension. 57 (6): 1026–1033. doi:10.1161/HYPERTENSIONAHA.111.169748. PMC 3105900. PMID 21536990.
- ^ Wallbach M, Koziolek MJ (September 2018). "Baroreceptors in the carotid and hypertension-systematic review and meta-analysis of the effects of baroreflex activation therapy on blood pressure". Nephrology, Dialysis, Transplantation. 33 (9): 1485–1493. doi:10.1093/ndt/gfx279. PMID 29136223.
- ^ a b Acelajado MC, Hughes ZH, Oparil S, Calhoun DA (March 2019). "Treatment of resistant and refractory hypertension". Circulation Research. 124 (7): 1061–1070. doi:10.1161/CIRCRESAHA.118.312156. PMC 6469348. PMID 30920924.
- ^ Dudenbostel T, Siddiqui M, Oparil S, Calhoun DA (June 2016). "Refractory hypertension: A novel phenotype of antihypertensive treatment failure". Hypertension. 67 (6): 1085–1092. doi:10.1161/HYPERTENSIONAHA.116.06587. PMC 5425297. PMID 27091893.
- ^ "Blood Pressure". World Health Organization. Archived from the original on 18 April 2017. Retrieved 22 April 2017.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ^ Leng B, Jin Y, Li G, Chen L, Jin N (February 2015). "Socioeconomic status and hypertension: a meta-analysis". Journal of Hypertension. 33 (2): 221. doi:10.1097/HJH.0000000000000428. ISSN 0263-6352. PMID 25479029.
- ^ Petrie JR, Guzik TJ, Touyz RM (May 2018). "Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms". The Canadian Journal of Cardiology. 34 (5): 575–584. doi:10.1016/j.cjca.2017.12.005. PMC 5953551. PMID 29459239.
- ^ Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D (March 1995). "Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991". Hypertension. 25 (3): 305–313. doi:10.1161/01.HYP.25.3.305. PMID 7875754. S2CID 23660820.
- ^ a b Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, Brown C, Roccella EJ (July 1995). "Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991". Hypertension. 26 (1): 60–69. doi:10.1161/01.HYP.26.1.60. PMID 7607734. Archived from the original on 20 December 2012.
- ^ Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S (July 2007). "Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004". Journal of the American Geriatrics Society. 55 (7): 1056–1065. doi:10.1111/j.1532-5415.2007.01215.x. PMID 17608879. S2CID 27522876.
- ^ a b c Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. (February 2010). "Heart disease and stroke statistics – 2010 update: a report from the American Heart Association". Circulation. 121 (7): e46–e215. doi:10.1161/CIRCULATIONAHA.109.192667. PMID 20019324.
- ^ Frohlich ED (October 2011). "Epidemiological issues are not simply black and white". Hypertension. 58 (4): 546–547. doi:10.1161/HYPERTENSIONAHA.111.178541. PMID 21911712.
- ^ Falkner B (July 2010). "Hypertension in children and adolescents: epidemiology and natural history". Pediatric Nephrology. 25 (7): 1219–1224. doi:10.1007/s00467-009-1200-3. PMC 2874036. PMID 19421783.
- ^ Luma GB, Spiotta RT (May 2006). "Hypertension in children and adolescents". American Family Physician. 73 (9): 1558–1568. PMID 16719248. Archived from the original on 26 September 2007.
- ^ "Global health risks: mortality and burden of disease attributable to selected major risks" (PDF). World Health Organization. 2009. Archived (PDF) from the original on 14 February 2012. Retrieved 10 February 2012.
- ^ Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (December 2002). "Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies". Lancet. 360 (9349): 1903–1913. doi:10.1016/S0140-6736(02)11911-8. PMID 12493255. S2CID 54363452.
- ^ Singer DR, Kite A (June 2008). "Management of hypertension in peripheral arterial disease: does the choice of drugs matter?". European Journal of Vascular and Endovascular Surgery. 35 (6): 701–708. doi:10.1016/j.ejvs.2008.01.007. PMID 18375152.
- ^ a b c d e f g h Esunge PM (October 1991). "From blood pressure to hypertension: the history of research". Journal of the Royal Society of Medicine. 84 (10): 621. doi:10.1177/014107689108401019. PMC 1295564. PMID 1744849.
- ^ a b Kotchen TA (October 2011). "Historical trends and milestones in hypertension research: a model of the process of translational research". Hypertension. 58 (4): 522–38. doi:10.1161/HYPERTENSIONAHA.111.177766. PMID 21859967.
- ^ Postel-Vinay N, ed. (1996). A century of arterial hypertension 1896–1996. Chichester: Wiley. p. 213. ISBN 978-0-471-96788-0.
- ^ Heydari M, Dalfardi B, Golzari SE, Habibi H, Zarshenas MM (July 2014). "The medieval origins of the concept of hypertension". Heart Views. 15 (3): 96–98. doi:10.4103/1995-705X.144807. PMC 4268622. PMID 25538828.
- ^ Emtiazy M, Choopani R, Khodadoost M, Tansaz M, Dehghan S, Ghahremani Z (2014). "Avicenna's doctrine about arterial hypertension". Acta medico-historica Adriatica. 12 (1): 157–162. PMID 25310615.
- ^ Swales JD, ed. (1995). Manual of hypertension. Oxford: Blackwell Science. p. xiii. ISBN 978-0-86542-861-4.
- ^ Wilking SV (16 December 1988). "Determinants of Isolated Systolic Hypertension". JAMA: The Journal of the American Medical Association. 260 (23): 3451–3455. doi:10.1001/jama.1988.03410230069030. ISSN 0098-7484. PMID 3210285.
- ^ "1993 guidelines for the management of mild hypertension: memorandum from a WHO/ISH meeting". Bulletin of the World Health Organization. 71 (5): 503–517. 1993. ISSN 0042-9686. PMC 2393474. PMID 8261554.
- ^ a b Dustan HP, Roccella EJ, Garrison HH (September 1996). "Controlling hypertension. A research success story". Archives of Internal Medicine. 156 (17): 1926–1935. doi:10.1001/archinte.156.17.1926. PMID 8823146.
- ^ Lyons HH, Hoobler SW (February 1948). "Experiences with tetraethylammonium chloride in hypertension". Journal of the American Medical Association. 136 (9): 608–613. doi:10.1001/jama.1948.02890260016005. PMID 18899127.
- ^ Bakris GL, Frohlich ED (December 1989). "The evolution of antihypertensive therapy: an overview of four decades of experience". Journal of the American College of Cardiology. 14 (7): 1595–1608. doi:10.1016/0735-1097(89)90002-8. PMID 2685075.
- ^ Novello FC, Sprague JM (1957). "Benzothiadiazine dioxides as novel diuretics". J. Am. Chem. Soc. 79 (8): 2028–2029. doi:10.1021/ja01565a079.
- ^ a b Chockalingam A (May 2007). "Impact of World Hypertension Day". The Canadian Journal of Cardiology. 23 (7): 517–519. doi:10.1016/S0828-282X(07)70795-X. PMC 2650754. PMID 17534457.
- ^ Chockalingam A (June 2008). "World Hypertension Day and global awareness". The Canadian Journal of Cardiology. 24 (6): 441–444. doi:10.1016/S0828-282X(08)70617-2. PMC 2643187. PMID 18548140.
- ^ Alcocer L, Cueto L (June 2008). "Hypertension, a health economics perspective". Therapeutic Advances in Cardiovascular Disease. 2 (3): 147–155. doi:10.1177/1753944708090572. PMID 19124418. S2CID 31053059.
- ^ Elliott WJ (October 2003). "The economic impact of hypertension". Journal of Clinical Hypertension. 5 (3 Suppl 2): 3–13. doi:10.1111/j.1524-6175.2003.02463.x. PMC 8099256. PMID 12826765. S2CID 26799038.
- ^ Coca A (2008). "Economic benefits of treating high-risk hypertension with angiotensin II receptor antagonists (blockers)". Clinical Drug Investigation. 28 (4): 211–220. doi:10.2165/00044011-200828040-00002. PMID 18345711. S2CID 8294060.
- ^ Taylor SS, Sparkes AH, Briscoe K, Carter J, Sala SC, Jepson RE, Reynolds BS, Scansen BA (March 2017). "ISFM Consensus Guidelines on the Diagnosis and Management of Hypertension in Cats". Journal of Feline Medicine and Surgery. 19 (3): 288–303. doi:10.1177/1098612X17693500. PMID 28245741.
- ^ a b Acierno MJ, Brown S, Coleman AE, Jepson RE, Papich M, Stepien RL, Syme HM (November 2018). "ACVIM consensus statement: Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats". Journal of Veterinary Internal Medicine. 32 (6): 1803–1822. doi:10.1111/jvim.15331. PMC 6271319. PMID 30353952.
Further reading
[edit]- 2023 ESH guideline: Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, et al. (1 December 2023). "2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA)". Journal of Hypertension. 41 (12): 1874–2071. doi:10.1097/HJH.0000000000003480. ISSN 1473-5598. PMID 37345492.
- 2022 AAFP guideline: Coles S, Fisher L, Lin KW, Lyon C, Vosooney AA, Bird MD (December 2022). "Blood Pressure Targets in Adults With Hypertension: A Clinical Practice Guideline From the AAFP". American Family Physician. 106 (6): Online. ISSN 1532-0650. PMID 36521481. Key recommendations.
- 2019 NICE guideline: "Hypertension in adults: diagnosis and management". National Institute for Health and Clinical Excellence (NICE). 28 August 2019.
- 2018 ESC/ESH guideline: Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. (1 September 2018). "2018 ESC/ESH Guidelines for the management of arterial hypertension". European Heart Journal. 39 (33): 3021–3104. doi:10.1093/eurheartj/ehy339. PMID 30165516.
- 2017 ACC/AHA guideline: Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, et al. (15 May 2018). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults". Journal of the American College of Cardiology. 71 (19): e127–e248. doi:10.1016/j.jacc.2017.11.006. PMID 29146535.
- 2014 JNC 8 guideline: James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. (February 2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
Cardiovascular disease (vessels) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Arteries, arterioles and capillaries | |||||||||
| Veins |
| ||||||||
| Arteries or veins | |||||||||
| Blood pressure |
| ||||||||